The Hartford Foundation’s Continued Commitment to Geriatric Medicine
The Hartford Foundation has made a long-term commitment to develop the medical school faculty needed to improve health care for older Americans. Through the Centers of Excellence in Geriatric Medicine and Training initiative, hundreds of junior faculty and fellows in geriatrics have been trained, promising new research is underway, geriatrics education in medical schools has expanded, and the prestige and prominence of the field of geriatrics has been raised. But more work remains to be done, and the Center of Excellence program continues to evolve to meet the challenges ahead.

Jennifer Kapo, MD, Assistant Professor examining patient, George E. Moody with Jerry Johnson, MD, University of Pennsylvania Center of Excellence. Dr. Kapo was awarded a Hartford Academic Fellowship in 2001.
Building on the success of the Centers of Excellence Initiative, the Foundation has identified additional areas where funding will further enhance the program’s impact. For example, each of the 24 Hartford Centers of Excellence has independently developed a model to use funds to best serve the goals of faculty recruitment
and development within the context of the individual medical center. Through this process, each Center has learned valuable lessons and developed techniques for recruiting and training future geriatric leaders. But this information has not been systematically shared with other Centers of Excellence or with the wider community of academic medical centers.
The Hartford Center of Excellence Network Resource Center was funded in 2005 to facilitate information exchange among the centers and to disseminate the Centers’ best practices to the academic community. The Network Resource Center has begun the development of a best practices inventory, collecting descriptions of model programs from Centers of Excellence directors. By identifying these best practices and preparing comprehensive descriptions, the Network Resource Center will serve as a hub of information for all Centers of Excellence directors. In the following years, the Network Resource Center will produce topical papers on current issues in academic geriatrics development and recruitment using the experiences of the Centers of Excellence in their role as the country’s exemplar programs in geriatric faculty development. The papers will be disseminated to Centers of Excellence program directors and members of the Association of Directors of Geriatric Academic Programs.
The Hartford Foundation recognizes the need to improve health care systems so older adult patients benefit from the innovations in aging research and geriatric medicine that are generated in academic centers. To encourage medical centers to develop model systems of geriatric care, the Foundation launched the Centers of Excellence Clinical Service Initiative. Five Centers of Excellence were awarded challenge grants for projects aimed at improving systems for delivering care to geriatric patients. By fostering innovation in health care delivery, these centers also position themselves to increase recruitment of students and residents to careers in geriatric medicine. The projects address diverse clinical needs, targeting a variety of health care settings across the continuum of care. Starting in 2006, each of the five centers will receive $155,000 for two years to develop these new venues of care.
Center of Excellence Clinical Services Challenge Grants
Advances in aging research and geriatric medicine will ultimately improve health care for the elderly only if systems are in place to translate new medical knowledge into every day clinical practice. The Hartford-designated Centers of Excellence are ideally positioned to serve as productive laboratories for testing new ways to structure and deliver health care to older patients.
In 2005, five Centers of Excellence received two-year challenge grants to jump-start the development of new models to improve clinical care for older adults, as well as to improve the training of future physicians, nurses and other team members.
Boston Medical Center, Boston, Massachusetts
Redesigning Long-Term Care Services for Urban Vulnerable Elders
Boston University (BU) Geriatric Services cares for 2,500 patients in its integrated system of care, which includes an ambulatory practice, home care program, nursing home program and inpatient service. Funds from the Hartford Foundation will support costs to redesign care provided to local residents to reduce the use of the emergency department, which will reduce the frequency of ambulance diversion from its emergency room.
Johns Hopkins University, Baltimore, Maryland
Geriatric Floating Interdisciplinary Team
Johns Hopkins University is using its Hartford Foundation grant to implement the Geriatric Floating Interdisciplinary Team, a new model of geriatric hospital care for older adults. This model of care is intended to improve the safety and efficiency of care and care transitions within the hospital and after discharge to a post-acute care setting. Mechanisms are being developed to identify and track frail elders upon admission and after discharge, which include educating patients and families about managing transitions and ensuring that patientsí goals and essential information are transmitted to appropriate new providers with each care transition.
Mount Sinai Medical Center, New York, New York
The Four “C’s” of Excellent Geriatric Hospital Care: Coordination, Collaboration, Communication, Continuity
Mount Sinai Medical Center plans to implement its Four “C’s” intervention in their 34-bed Acute Care of Elders (ACE) unit. The grant will support training and staff time to assist internal medicine residents with responsibilities such as completing discharge summaries, making post-discharge telephone calls, and determining whether
admission might have been prevented, to help future doctors understand the effects of hospitalization on the overall health of older patients.
University of California, Los Angeles
Redesigning a Geriatrics Practice to Manage Chronic Conditions
This grant addresses the need to improve the effectiveness and efficiency of outpatient care for frail older adults with multiple health problems. Focusing on five conditions (falls, urinary incontinence, dementia/cognitive impairment, depression and heart failure), medical trainees will learn chronic disease management and nurse practitioner trainees will observe new models of professional practice. All students will be exposed to interdisciplinary teamwork and will become familiar with use of an electronic health record to manage chronic disease.
University of California, San Francisco
Going Home
The “Going Home” project was created to improve hospital care and the care patients receive as they move among different sites of care, and especially as they are discharged from a health care facility to go home. It focuses on the goals of patients and families for safe and independent living and uses home visits as a teaching venue. It involves an interdisciplinary team of practitioners from geriatrics, hospital medicine, nursing, pharmacy and social work.
Finally, the Hartford Foundation has expanded the Centers of Excellence in Geriatric Medicine and Training Initiative to include geriatric psychiatry. An important component of the capacity to provide quality health care to older adults is the ability to meet their mental health needs. Yet a critical shortage of geriatric psychiatrists threatens to deny many older people the mental health care services they need. As with geriatric medicine, rectifying this requires increasing the number and quality of physician faculty specializing in geriatric psychiatry. Because physicians pursuing an academic career in geriatric psychiatry face similar obstacles as those in academic geriatric medicine, the Hartford Foundation is using the Centers of Excellence approach to bolster geriatric psychiatry faculty development. Two Centers of Excellence in Geriatric Psychiatry have been designated: University of California, San Diego and University of Pittsburgh.
San Diego is creating a Center of Excellence in Geriatric Psychiatry to train a new generation of geriatric psychiatrists and physician-researchers to meet the needs of older persons with illnesses ranging from depression to psychotic disorders such as schizophrenia. “With the Hartford Foundation grant and establishment of the
Center of Excellence in Geriatric Psychiatry, we will be able to provide positive role models for promising psychiatric researchers, develop award programs and affinity groups, share resources, make programs sensitive to trainees’ practical needs, and assist individuals with the transition to an academic career,” says the Center’s director Dilip Jeste, MD, Estelle and Edgar Levi Chair in Aging and professor of psychiatry and neurosciences.
26 Centers of Excellence
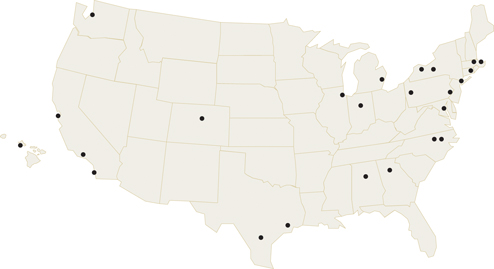 Baylor College of Medicine
Baylor College of Medicine
Boston University
Cornell University
Duke University
Emory University (Southeast CoE)
Indiana University
Harvard University
Johns Hopkins University
Mount Sinai School of Medicine
University of Alabama (Southeast CoE)
University of California, Los Angeles
University of California, San Diego, (Geriatric Psychiatry)
University of California, San Francisco
University of Chicago
University of Colorado
University of Hawaii
University of Michigan
University of North Carolina Chapel Hill
University of Pennsylvania
University of Pittsburgh
University of Pittsburgh (Geriatric Psychiatry)
University of Rochester
University of Texas Health Science Center at San Antonio
University of Washington
Yale University
The University of Pittsburgh’s Department of Psychiatry already trains nearly 20 percent of the academic geriatric psychiatrists now working in the United States. Through the Hartford Center of Excellence, the university continues to train future geriatric psychiatrists to specialize in research and physician education. “The importance of training physician educators can not be overstated,” says Center director Charles F. Reynolds III, MD, professor of psychiatry, neurology and neuroscience, University of Pittsburgh School of Medicine. “Now and in the future, a primary care doctor will be the first point of entry for elderly who seek treatment for mental illness. It is critical that these doctors receive specialized training in identifying and treating mental illness in this population.”
In December 2005, the Trustees of the Hartford Foundation reviewed and approved a strategic plan to continue and refine the Centers of Excellence initiative. Recognizing that American medical education is, at current rates, still several decades away from being able to adequately prepare all doctors for the patient demographics in the society in which they will practice medicine, the Foundation has recommitted to the Centers of Excellence initiative. New and renewal grants, beginning in 2006, will provide incentives to focus on recruitment into geriatric medicine, provide for longer grant awards in order to help further stabilize academic medicine, require leadership and management training for program participants, and provide support to senior faculty at Centers of Excellence when they are recruited to lead their own geriatric development programs. Recognizing society’s immense need for this work, the Foundation will continue to seek out funding partners to support this work, as well. Cumulatively, the Centers of Excellence in Geriatric Medicine and Training and the Foundation and its funding partners are preparing for the time when older patients routinely receive the health care that meets their needs efficiently and respectfully.
