Centers of Excellence: Support for Clinical Research
For geriatric researchers wishing to work with people to advance therapies and processes of care, clinical research is the career path. Clinical researchers work with human subjects-both well and ill older persons-to advance knowledge in aging research and geriatric medicine. They are committed to understanding the physiology of the body as it ages and the diseases that can impair functioning. They develop or test promising therapies and diagnostics to see how they work in actual patients and investigate clinically relevant research questions. Some clinical researchers take drugs or other therapies developed in a basic science lab and figure out how to apply this new knowledge to the treatment of patients.
In some respects, clinical research can be more complex than basic research. For example, clinical research in geriatrics often must be multidisciplinary, combining expertise in both geriatrics and another medical specialty. For example, research on new treatments for breast cancer in older women would require collaboration
among oncologists and geriatricians.
Clinical researchers are generally expected to have teaching responsibilities, to treat patients, to go on rounds, and to lead new service innovations. They are also required to engage in ongoing research activities and to publish their findings in peer-reviewed publications. Many advanced fellows are required toearn their salary by seeing patients in the clinic, thus spending valuable time that could be devoted to research projects.
Funds from the Hartford Centers of Excellence provides salary support for fellows and junior faculty in geriatrics, thus freeing them from clinical and other responsibilities and allowing them to concentrate on their research and scholarly development in academic geriatrics.
Searching for Biomarkers of Breast Cancer
“Cancer patients on TV may all look 40, but the fact is that cancer is really a disease of older people,” says Pearl H. Seo, MD, MPH, Associate, Divisions of Geriatrics and Medical Oncology, Duke University Medical Center, Raleigh, North Carolina. Dr. Seo’s original interest was in oncology because she was fascinated by the science. “To understand it fully you have to understand what’s happening at the cellular level,” she says. But exposure to geriatrics during her residency convinced her that even if she did oncology research, she would benefit from learning the clinical aspects of geriatric medicine, as well.
So Dr. Seo did a geriatrics fellowship at Harvard Medical School, where she studied quality of life in older men with prostate cancer. At Harvard she also met her husband, a North Carolina native. When he accepted a cardiology residency at Duke University, Dr. Seo joined the faculty at Duke with a primary appointment in geriatrics and a secondary appointment in medical oncology. She received Hartford junior faculty support beginning in July 2002 to research outcomes among older cancer patients.
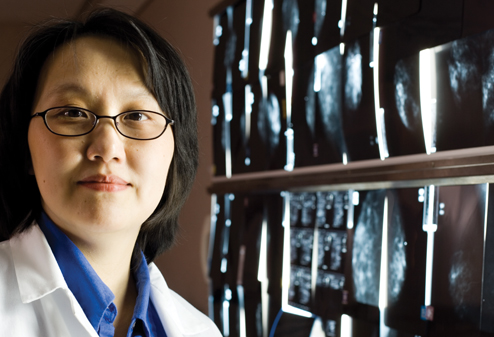
Pearl H. Seo, MD, MPH, Duke University Medical Center, Raleigh, NC. Because 63% of oncology patients are over the age of 65, cancer research needs to start addressing the health needs of older Americans. Beeson Scholar Dr. Seo was awarded NIA funding to include post-menopausal women in breast cancer research.
Dr. Seo and her colleagues at the Veterans Administration conducted a geriatric assessment questionnaire on 200 consecutive older men who came to the oncology and radiation clinics. “They were cancer survivors, but they had a lot of functional problems and co-morbidities,” says Dr. Seo. A three-year follow-up found that many of these patients complained of depression, pain, and anxiety. Dr. Seo and her associates found that oncologists and primary care doctors were able to effectively treat their cancer but failed to ask them about their emotional life.
During this time, Dr. Seo worked with a lot of female patients with breast cancer. “In the three years I did breast cancer clinical work I only saw patients older than 65,” she says. So, when she met Dr. Victoria Seewatldt, a researcher in the Duke Comprehensive Cancer Center investigating biomarkers of breast cancer in premenopausal women, Dr. Seo discussed the possibility of broadening the research population to include post-menopausal women, and in August 2005 received a five-year Paul B. Beeson/NIA K08 Career Development Award for the project PPARgamma: Biomarker for Breast Cancer in Older Women.
Currrently working with Jeffrey Marks, PhD, the two researchers are analyzing tissue samples to look for biologic predictive markers of breast cancer development in older women. This requires performing aspiration of the breast in high risk women. Because of the invasiveness of this procedure, Dr. Seo is determining if the same biologic information can be obtained from blood samples. “This is my foray into translational medicine, where I have to bridge the clinical side with the bench side,” says Dr. Seo.
If a blood marker of breast cancer can be found, it may provide useful information for better tailoring of treatment, predicting whether a specific form of chemotherapy will result in the best outcome, thus sparing the patient trials of ineffective therapies.
Having the Hartford junior faculty support was a great opportunity for Dr. Seo, who will continue her work in the field of translational breast cancer research in older women. “I’ve been able to do less clinical work and to invest more time in research and to meet people outside of my division,” she says. “As junior faculty it’s often difficult to make connections, especially outside of your division. Here, there’s a commitment to growth and to mentorship. It’s a treasure to have this.”
Why Does Alzheimer's Disease Disproportionately Affect African-Americans?
“I was born in Haiti, and I am very interested in cross cultural health, particularly the question of why African-Americans have two times the incidence of Alzheimer’s disease as Americans of European descent,” says Marie-Florence Shadlen, MD, Assistant Professor, University of Washington School of Medicine, Department of Medicine, Division of Gerontology and Geriatric Medicine.
Dr. Shadlen took a circuitous route to the field of geriatric research. She completed her fellowship in geriatrics at Stanford University in 1990, after which she began her career as a clinician teacher in geriatrics and a medical director of an Alzheimer's unit. According to Dr. Shadlen, this career choice was a good fit with her roles as both mother and physician. As her children got older, she turned her focus to professional interests and career advancement. But without a track record in research it was difficult for her to get started.

Marie-Florence Shadlen, MD, University of Washington, Seattle,WA, with patient. Dr. Shadlen was able to make a career change from clinician teacher to NIH-funded physician scientist with support from the Center of Excellence.
A move to the University of Washington in Seattle brought Dr. Shadlen to the attention of Itamar Abrass, MD, Professor and Division Head, University of Washington School of Medicine, Department of Medicine, Division on Gerontology and Geriatric Medicine. Dr. Abrass is the director of the Hartford Foundation Center of Excellence at the University of Washington, and is responsible for recruiting senior fellows and junior faculty into the program.
“We admit only two to four fellows each year,” he says. “We pick individuals who we think have the potential to ultimately develop a leadership role in geriatrics. We recruit the best people and then allow them to decide what excites them. Dr. Shadlen was interested in converting from a clinician teacher to a physician scientist. She came to our division to gain her scholarly experience.”
What excited Dr. Shadlen was epidemiologic research in Alzheimer’s disease and the epidemiology of dementia. She wanted to discover what, if any, biological or socioeconomic factors underlie the increased incidence of Alzheimer’s disease in African-Americans. It’s known that conditions such as diabetes, hypertension, and stroke are general risk factors for Alzheimer’s disease, and also there is a higher prevalence of these conditions in African-Americans. Dr. Shadlen wanted to find out if this might explain the greater risk for Alzheimer’s disease.
“We found that there doesn’t seem to be as clear a story as people assume on the effect on Alzheimer’s based on whether someone has diabetes, hypertension, or history of stroke,” she says. “This would have been an easy explanation and a good one for public health because it would mean there are clear prevention strategies.” Instead, Dr. Shadlen identified socioeconomic factors as being more important, particularly as it relates to education.
With a 2003 career development award from NIH entitled Social Factors and Epidemiology of Cognitive Decline, Dr. Shadlen is currently pursuing this line of research. She says that her successful switch to clinical research would not have been possible without the Hartford Foundation. “You need a track record to get funding, so they will feel you’re a worthy investment,” she says.
Why Do Older Patients Lose Weight?
“Without the Center of Excellence funding I would be back in practice because I wouldn’t have had the time to write my grant proposals and do the work that was necessary to get my research career started,” says Michi Yukawa, MD, MPH, Assistant Professor, Department of Medicine, Division of Gerontology and Geriatric Medicine, University of Washington, Seattle. Instead of returning to private practice, Dr. Yukawa, who did her fellowship training (1998-2000) at the University of Washington School of Medicine, spends her time engaged in clinical research, trying to understand why older people lose weight.
Dr. Yukawa's residency training was in traditional internal medicine, after which she joined a group practice. She found that most of her patients were elderly. Yet during her training she had received little exposure to geriatrics. "I wanted to be more competent in taking care of these complicated geriatric patients," she says. This led to her decision to do a fellowship in geriatrics, which sparked her career change from clinical practice to clinical research.
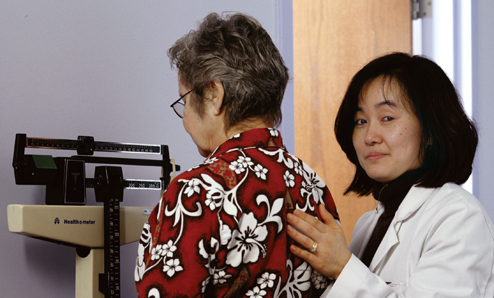
Michi Yukawa, MD, MPH, University of Washington, Seattle, WA, with patient. Sudden loss of appetite can lead to a dramatic decline in the health of older adults. Dr. Yukawa explores the causes and treatment strategies to prevent unexplained weight loss.
While seeing patients, Dr. Yukawa noticed that many of the older patients would suddenly lose their appetite and consequently lose weight, beginning a downward health spiral. “I couldn’t understand why somebody would all of a sudden not want to eat anymore,” she says. “There isn’t a good understanding of why this happens, and how best to treat it.”
Dr. Yukawa decided to investigate the reasons for unexplained weight loss in older adults. In order to do this research, she initiated a collaboration with the Division of Endocrinology. “Endocrinology was one of my least favorite subjects in medical school,” she says. “Ironically, now that’s all I do.” She now has mentors in both the Division of Endocrinology and the Division of Gerontology and Geriatric Medicine.
She began by looking at healthy older adults. She had them lose a small amount of weight and then observed how long it took them to gain the weight back, as compared to a group of younger adults. She recorded hormone levels in her patients, trying to determine if hormones impact older adults differently than their younger counterparts. For example, leptin is a protein hormone that helps the body regulate food intake and energy use and may help the body feel “full” after eating. And ghrelin is a hormone produced in the stomach that stimulates appetite. Both may help to explain why older patients have a harder time maintaining or gaining weight. For the most part, healthy older adults do not regain weight after losing a small amount. Dr.Yukawa is now conducting similar studies with patients who are not as healthy.
How does she like clinical research with geriatric patients? “It’s fun, frustrating at times. But most of the time, it’s very rewarding to work with older people,” she says. In 2003, Dr. Yukawa received a five-year career development award to study “Body Weight Regulations of Older Adults” from the NIH.
