2012 ANNUAL REPORT
Health Care Cost and Quality (1979-1994)
As rising health care costs grew into a major public concern in the 1970s, the Hartford Foundation responded with funding initiatives in Health Care Cost and Quality. These initiatives supported innovative models of reimbursement, as well as cost containment systems such as HMOs. Later, the Foundation would widen its focus to include the delivery of high-quality care within these cost-saving models.
By the mid-1990s, Congress defeated White House plans to overhaul the U.S. health care system and political and economic conditions proved resistant to change. As a result, the Foundation Trustees re-evaluated their funding strategy and decided to end work in Health Care Cost and Quality, while expanding the Aging and Health program. A number of successful cost and quality projects would either have enduring impact or live on in the Aging and Health program. For example:
- A grant to Donald M. Berwick, MD, a future administrator of the Centers for Medicare and Medicaid Services, helped launch the Institute for Healthcare Improvement (IHI). This organization has become a major force in health care delivery reform. IHI has mobilized 100,000 individuals in quality improvement work and developed the “triple aim” framework for increasing quality and patient satisfaction, improving population health, and reducing costs. Dr. Berwick’s idea for IHI proved so popular among health systems interested in improving quality and safety that he offered to return the Foundation’s start-up funds (an offer not accepted).
- A grant project headed by John E. Wennberg, MD, MPH, at the Dartmouth Institute for Health Policy and Clinical Practice, examined variations in physicians’ practices in areas across the country as a way to understand rising health care costs. This work continues to be significant today. Geographic variations in Medicare expenditures have focused policy makers’ attention on reducing “hot spots” of high cost/low quality care and helped frame much of the debate for the 2010 passage of the Affordable Care Act.
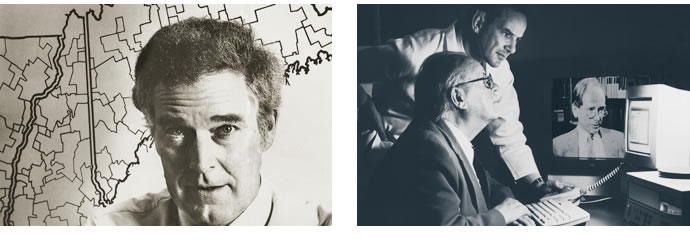
(Picture Above Left) John E. Wennberg, MD, MPH, at the Dartmouth Institute for Health Policy and Clinical Practice identified geographic variations in the way physicians treat similar conditions. He found that higher costs do not necessarily produce better outcomes for patients.
(Right) Dr. Wennberg and his colleagues created computer-controlled videos to help patients consider the risks and benefits of different treatment options. A doctor and patient review a prototype video.
- An organization called On Lok, in San Francisco, CA, created a cost-saving model of health care delivery more generally known as the Program of All-Inclusive Care for the Elderly (PACE). The program provides services to older adults that allow them to continue living independently. Today PACE is an effective model for integrating Medicare and Medicaid financing and high-quality care delivery for poor, frail older adults. One of the original project leaders, Jennie Chin Hansen, RN, is now the CEO of the American Geriatrics Society, a current Foundation grantee.
- Paul D. Clayton, PhD, a national leader in health informatics innovation (then at Columbia University), received Hartford funding to explore information technology in the delivery of care and maintenance of patient health records. Dr. Clayton subsequently received a grant under the Foundation’s Aging and Health program to use health information technology to create innovative primary care service delivery to elders. Dr. Clayton also mentored David A. Dorr, MD, MS, a geriatrician and health care informaticist, who continues to refine and spread the model (Care Management Plus).