 Last week on Health AGEnda, I stuck up for the Center for Medicare and Medicaid Innovation (CMMI) in the face of what seemed to me fairly unrealistic criticism from a Wall Street Journal op-ed.
Last week on Health AGEnda, I stuck up for the Center for Medicare and Medicaid Innovation (CMMI) in the face of what seemed to me fairly unrealistic criticism from a Wall Street Journal op-ed.
I approached the issue from my perspective as a funder and as a very, very, much smaller player in the reform of the health care delivery system than CMMI. It got me thinking that, while I have offered advice directly to the Centers for Medicare and Medicaid Services (CMS) and CMMI staff and mentioned various concerns here on the blog in passing, I haven’t really tried to think through what our experience at Hartford suggests might help CMMI be as effective as possible.
CMMI is the big player in health care delivery reform—the changes to culture, training, regulation, payment, and organization in health care that we all hope will lead to higher quality care, a healthier public, and lower costs of care per capita.
CMMI is the new office within CMS created as part of the Affordable Care Act (ACA) with a mission of leading the reform and improvement of health care in the United States. It was granted $10 billion dollars to be spent over 10 years, which—while I do not believe is enough—is certainly more than had previously been spent by CMS’ Office of Research, Development, and Information (ORDI) and the Agency for Healthcare Research and Quality (AHRQ) put together.
So it is the big player in health care delivery reform—the changes to culture, training, regulation, payment, and organization in health care that we all hope will lead to higher quality care, a healthier public, and lower costs of care per capita.
As I’ve been thinking about my recommendations, I also realize that we have not always lived up to these standards ourselves. But if only those without sin are allowed to throw stones, we won’t be able to make much progress.
So here goes . . .
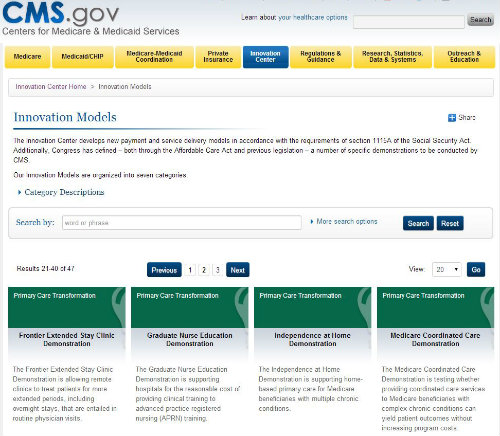
1. Share details on funded projects. It is inappropriate for publicly funded health care innovation projects to be kept secret at any stage. The funded proposals, interim and final reports and evaluations, and eventually all the data collected from funded projects should be made available.
This standard, which is already applied to science projects funded by the National Institutes of Health, facilitates the exchange of ideas and speeds innovation. CMS and CMMI treat too much work as proprietary to applicants and keeps too much of evaluators’ results confidential too long. The lack of openness and communication prevents projects from building upon one another and improving, and allows flat tires to be reinvented over and over again.
The CMMI website emphasizes some interesting mapping software, but it is much less useful in finding out what the clinical and financial results are of its important investments.
I’m sure that changes to the operating rules of innovation awards, contracts, and cooperative agreements would require substantial regulatory and even legislative changes, but it would be worth it.
2. Conduct evaluations and make results available in a timely fashion and with an eye on big-picture lessons. Looking at the reports on Medicare demonstrations started under the Medicare Modernization Act (MMA) of 2003 on the CMS/CMMI website, I see a great deal of out-of-date and incomplete information. For example the page reporting on the disastrous MMA section 721 “Medicare Health Support” demonstration, which involved development and testing of chronic care improvement programs for people with multiple chronic illnesses, reads:
“The programs were overseen by the Centers of Medicare and Medicaid Services (CMS) and operated by health care organizations chosen through a competitive selection process. Phase I program operations began between August 2005 and January 2006. Phase I ended on August 31, 2008 and CMS is assessing the results of this program.”
The program is long since over, the evaluation contract is long since over, and there will be no further reports. But this is one of the largest health services demonstrations ever, so it is probably time to do a real, long-term look back and extract all the painful lessons possible not only about the clinical models and the evaluation methodology, but also about the application, selection, contracting, and monitoring process.
The history of Medicare demonstrations and all of the other research work in the area, public and private, is rich, complex, and relevant to what CMMI is doing today.
I think it is perhaps even more important that there be feedback available on the little- known Multi-payer Advanced Primary Care Initiative. This project is the first of several Medicare medical home-type demonstrations, started just before the ACA was passed. The last sites in the demo were started in January 2012, and so must have more than two years of experience to report.
How can there be no results, reports, case studies, or even commentary available to inform the younger Comprehensive Primary Care Initiative and the FQHC Advanced Primary Care Practice Demonstration, mandated in the ACA, much less all of the private medical home/health home initiatives that seem to pop up everywhere?
I am very concerned that the success rate among the Innovation Challenge Grants will be disappointingly low and that the information captured will be limited and the lessons few.
3. Take a more strategic approach to grantmaking. While the two rounds of the Health Care Innovation Awards will only total $2 billion or so (20 percent of CMMI’s 10-year allocation), I doubt anyone is happy with the process or that the results will be as good as they should be.
I’ve followed the process closely, supporting grantee applications in the first round and serving as a reviewer in the second. Both rounds of applications and reviews were hurried and conducted without sufficient information or support. At the John A. Hartford Foundation, we often go through multiple rounds of critiques and proposal revisions with potential grantees to be sure they are using the best methods, the best ideas, and the appropriate resources for their projects.
Even with a strong grantmaking process that helps applicants include the best current evidence to give them the best chance to succeed, the odds don’t get much above 50-50. While not every demonstration should work, they should all contribute meaningfully to the next round of innovation, with methods that are appropriate to the questions being asked. I am very concerned that the success rate among the Innovation Challenge Grants will be disappointingly low and that the information captured will be limited and the lessons few.
I think groups of grants around a few common themes would have been a better compromise between a bottom-up competition of ideas and the top-down guidance of experience. Even if there would have been fewer happy grantees, we would probably learn more.
Innovations can’t be expected to spring like Athena fully formed from the head of Zeus. They need feedback and adjustment to get to their best performance. And to do that, they need information.
4. Invest in infrastructure. In every recent demonstration I know of, CMS/CMMI grantees have complained about a failure to get Medicare claims data in a timely and useful way to facilitate working with patients. Perhaps it is a convenient excuse for the many disappointing results, but I suspect there is truth to it.
We have to be able to get information that is more reliable and more timely to understand not only if our innovations are working, but to answer more nuanced questions, such as for whom are they working and how much are they working?
Innovations can’t be expected to spring like Athena fully formed from the head of Zeus. They need feedback and adjustment to get to their best performance, and to do that, they need information.
From the other side of the funder-grantee table, I doubt CMS/CMMI has ever felt fully informed as to what “exactly” an intervention really is doing—what is inside the proverbial “black box.”
Getting accurate, real-time monitoring of work processes, however, is really important if you want to create a benefit for all Medicare providers to use. You need to know how much it costs to deliver some new model of care, by what kind of staff, and what kinds of documentation is enough—but not more than is really needed—to assess the appropriateness of the care process. If an innovation works, you have to be prepared for success with all the tools needed to spread the model.
One of my most serendipitous experiences as a funder was supporting (against my better judgment) the creation of an on-line performance tracking tool for our depression in primary care demonstration, Project IMPACT. Not only did this tool allow the project to fairly inexpensively describe the process steps and contributors to the successful intervention, but it also grew to become a key support of sound clinical care as a decisions support and reminder tool.
CMS/CMMI needs to invest in some state-of-the-art tools to be able to learn at a micro level what its wide array of projects and grantees have to teach as they grapple with the complexities of changing health care.
CMMI’s heavy reliance on external consulting firms for project design and evaluations has many efficiencies and benefits, but it comes at the cost of developing more expertise internally.
5. Hiring more staff is critical. Returning to the points of my last post, far from being overstaffed at the 400+ FTE planned for next year, on a proportional basis to Hartford Foundation staffing, CMMI would have 800 staff members. Those extra staff are the key resource to spend more time with grantees to learn what they are doing, help them overcome inevitable obstacles, communicate with the public and the rest of government, absorb the lessons of the work, and improve.
CMMI’s heavy reliance on external consulting firms for project design and evaluations has many efficiencies and benefits, but it comes at the cost of developing more expertise internally.
I don’t know if this advice will be helpful or even welcome. I believe that CMMI has a very hard job and one that is very important to our country’s future and the health of older Americans, both now and the ones we aspire to be in the future.
If readers have suggestions to add or disagree with mine, please feel free to comment on the blog here or just email them to me directly.