Testing and implementing new approaches to better care.
For decades, we’ve built a field of experts in aging and health who are innovating and improving care.
We’re transforming the way people think about care for older adults by investing in what works.
—Terry Fulmer, PhD, RN, FAAN, President, The John A. Hartford Foundation

Age-Friendly Health Systems Initiative
We all deserve reliable health care that aligns with our goals and preferences, particularly as we get older. It’s not just the right thing to do, it’s an economic imperative. At the time that adults over age 65 were only 12 percent of the population, they accounted for 35 percent of all hospital stays and 26 percent of all doctor visits, and those trends continue. Poor-quality care harms older patients, causes families to suffer, and wastes money.
We know meaningful change requires bold action. In 2017, we launched the Age-Friendly Health Systems initiative in partnership with the Institute for Healthcare Improvement, the American Hospital Association, and the Catholic Health Association.
Together with experts in geriatric care, we are developing and testing an innovative model of care for older patients in five health systems across more than 30 states: Anne Arundel Medical Center, Ascension, Kaiser Permanente, Providence St. Joseph Health, and Trinity Health. Our goal: to bring age-friendly care to 20 percent of US hospitals and health systems by 2020.
In the first stage of the initiative, which runs from 2017 through 2018, we are testing the Age-Friendly Health System prototype and scaling the model with participating health systems. Our efforts in this initial phase center on high-level interventions, referred to as the 4M Bundle, which should be delivered across care settings, from the hospital to the kitchen table:
- What Matters: Know and act on each older adult’s specific health goals and preferences
- Medications: Use age-friendly medications that facilitate mobility, mentation, and “deprescribe” medications that aren’t age-friendly
- Mentation: Identify and manage depression, dementia, and delirium
- Mobility: Ensure that older adults move every day
The second stage of the project, to be launched in 2019, will spread the model to an additional 10 to 15 health systems. We will also continue efforts to scale up the model to more than 1,000 age-friendly hospitals and health systems by 2020.
A hospital like ours already had programs on elder care, but we never looked at it from a whole system approach. We’re now testing ideas and asking critical questions and it’s making a difference. When we feel like we can better care for our patients, there is a positive effect on clinicians.
—Barbara Jacobs, MSN, RN, Vice President, Nursing and Chief Nursing Officer, Anne Arundel Medical Center

Testing Patient Priorities Care
We are living longer than ever before, but that often comes with additional health care needs. One in five people in the US age 65 or older have three or more chronic conditions. As different clinicians manage these various conditions, care is often fragmented and confusing to patients and caregivers. This uncoordinated care can be unhelpful, burdensome, and even harmful: one in five Medicare beneficiaries experience “guideline-driven harm” as a result of clinicians prescribing disease-specific medications that adversely affect the patient’s coexisting conditions.
Patient Priorities Care is a new approach for care teams that uses patients’ own priorities to align health care among all their clinicians. The idea came to life in 2014, when a group of patients, clinicians, health system leaders, and other national experts proposed feasible strategies for improving the care of older adults with multiple chronic conditions.
The process begins with a member of the health care team who serves as a facilitator with the patient and his or her family, helping identify the patient’s health values and priorities. The care team translates the patient’s priorities into specific care options, explains any tradeoffs, and integrates care, including tests, self-care tasks, procedures, and medications. Over time, the team tailors care to help the patient meet his or her goals. The objective: less burdensome care that is more consistent with what matters most to the older adult.
In late 2016, we launched a pilot program at primary care practices in an Accountable Care Organization and its partner cardiology practices to test and build evidence about Patient Priorities Care and refine the approach. In 2017, the program enrolled nearly 200 older patients and a cadre of clinicians. The Patient Priorities Care team is conducting quantitative and qualitative analyses, such as patient interviews, to assess the model.
Evaluation results will be made public in 2018, but preliminary results find:
- Patients report a better understanding of what they want out of their health care and how to get there.
- Clinicians report having better communication with their clinician colleagues.
- Clinicians report care options were clarified resulting in more consistent care.
The John A. Hartford Foundation has been successful because of a combination of the passion that they have for improving care, the persistence they have shown over the years, and their astute assessment of opportunities that can help move us toward tangible improvements in care for older adults in this country.
—Mary Tinetti, MD, Chief of Geriatrics, Yale School of Medicine

National Collaboratory to Address
Elder Mistreatment
An estimated 10 percent of older adults—5 million people—suffer from elder abuse, neglect, self-harm, exploitation, and other forms of mistreatment each year. Health systems, often an entry point for older adults, have a golden opportunity to intervene. And yet, there is no standard protocol for identifying and treating older adults who have endured mistreatment.
In late 2016, we funded the National Collaboratory to Address Elder Mistreatment with the Education Development Center (EDC) to develop and pilot test a new standard for elder abuse interventions. The Collaboratory convened leading national experts in four geographically diverse states—California, Massachusetts, New York, and Texas—to create a prototype model for identifying and treating survivors of elder mistreatment that can work in emergency departments nationwide.
Collaboratory participants are making steady progress toward closing a critical gap in US health care delivery—the failure to identify and prevent elder mistreatment. The University of Southern California Keck School of Medicine/National Center on Elder Abuse, The University of Texas Health Science Center at Houston/Texas Elder Abuse and Mistreatment Institute, State of Massachusetts Executive Office of Elder Affairs, and New York’s Weill Cornell Medicine, Division of Geriatrics and Palliative Medicine are working together to create a replicable community-based, multi-disciplinary model for curbing abuse, neglect, self-harm and the exploitation of older people.
The model will be adaptable to communities big and small—including rural areas where the needs are especially high—and is expected to improve the way emergency department personnel work with older adults who come through their doors. By training all personnel in the department—from nurses to social workers—we are building a more informed workforce to identify abuse and neglect at the earliest stages.
The Foundation’s focus on eradicating elder abuse, neglect, and exploitation has been extraordinary. They are thinking about how older patients can be impacted by the health care system and are scaling up community-based models to identify and treat elder abuse and mistreatment, especially in low-resource areas. By bringing us together through a grant to EDC, we are collectively on the brink of real transformational change.
—Laura Mosqueda, MD, Dean, Keck School of Medicine, University of Southern California
Spreading what works.
We know our success relies on working with other organizations to accelerate improvements in care for older adults with complex health needs.

Sharing the Better Care Playbook
When people with complex medical and social needs require health care, they encounter a system that’s expensive, inefficient, and poorly coordinated across hospitals, physician practices, and other places where people go to receive care and supportive services. What’s more, the majority of these patients are older than age 65—elevating the need to address this issue as America’s population ages.
Six health care foundations—The John A. Hartford Foundation, The Commonwealth Fund, the Milbank Memorial Fund, the Peterson Center on Healthcare, the Robert Wood Johnson Foundation, and The SCAN Foundation—are working together to improve care for people with complex needs. Developed by experts at the Institute for Healthcare Improvement, the Better Care Playbook curates information on what’s worked to help this patient population, for use by health system leaders, insurers, policymakers, and others.
The Playbook has curated and shared dozens of key resources highlighting successful approaches for frail older adults, people living with serious illness, and other populations. New resources are continually added and cover a range of topics including building age-friendly health systems, developing serious illness strategies for health plans and accountable care organizations, and implementing home-based care to promote aging in place.
The John A. Hartford Foundation has a wealth of knowledge, experience, and familiarity with older adults who have complex health and social needs. Their insights have deeply informed the collective thinking of our collaboration around the Playbook to maximize its effectiveness.
—David Blumenthal, MD, President, The Commonwealth Fund

Spreading Home-Based Primary Care
There are approximately 6 million fragile, vulnerable older adults in the US with difficulty accessing office-based primary care because they are frail, functionally limited, and homebound. They are among the costliest patients due to a snowball effect from multiple chronic conditions, functional impairment, frailty, and social stressors.
Teams at the Johns Hopkins University School of Medicine and University of California, San Francisco (UCSF), in collaboration with the Home Centered Care Institute (HCCI) and the American Academy of Home Care Medicine are training clinicians in measuring and tracking the quality of care in home-based primary care, and in spreading information about how emerging payment models might sustain and expand access to this care.
In 2017, HCCI trained more than 120 clinicians and practice managers at prestigious institutions—including the Cleveland Clinic, University of Arizona Center on Aging, and UCSF, just to name a few—to perform home-based primary care. Beyond that, HCCI plans to train 5,000 clinicians and practice managers with the goal of ensuring that at least half of people who can benefit from home-based primary care have access to those services.
Home-based primary care provides better care and saves money. We want to bring it back to its rightful place in the fabric of our health system. The support of The John A. Hartford Foundation not only helps us accomplish the work, but also opens doors by letting potential partners know that they’re behind this.
—Thomas Cornwell, MD, Chief Executive Officer, Home Centered Care Institute

Supporting Family Caregivers
More than 18 million family members are taking care of older adults in the US, and nearly 9 million are caring for people with high needs like dementia. Many of these caregivers are themselves at risk for poor health, emotional stress, and financial harm, according to a National Academies of Sciences, Engineering, and Medicine report co-sponsored by The John A. Hartford Foundation. Families Caring for an Aging America recommends that health systems and clinicians should strengthen their capacity to recognize and support family caregivers, among other recommendations for addressing caregiver needs.
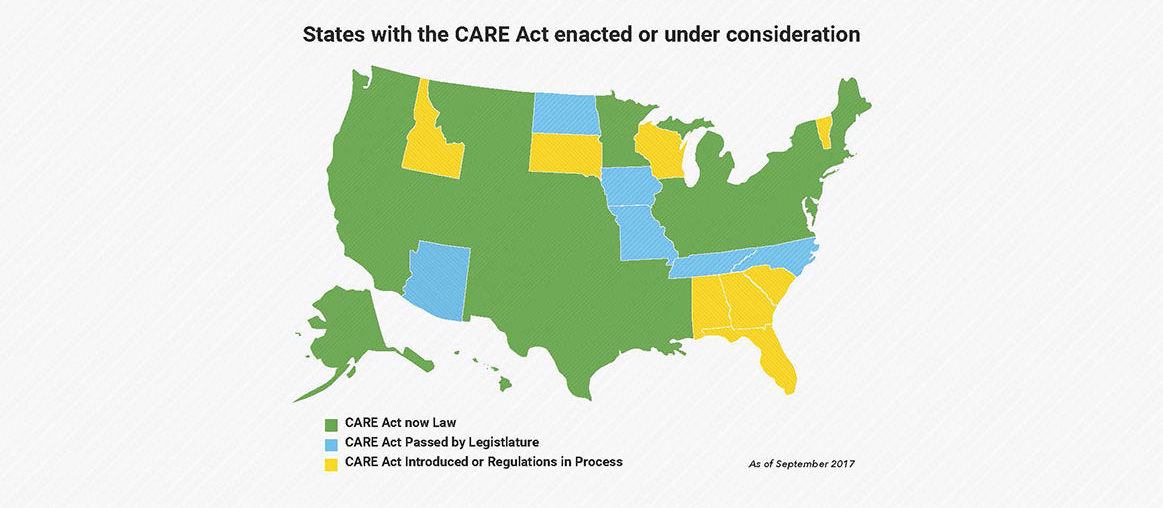
The Supporting Family Caregivers Providing Complex Care project—in partnership with AARP’s Home Alone Alliance—is helping health systems better serve family caregivers. The project will identify and share best practices in implementing the CARE Act, a law passed in 39 states that requires hospitals to identify and educate patients’ family caregivers before discharge. This project and others—such as the Dementia Care Program at the University of California, Los Angeles (UCLA) —also educate nurses and other clinicians to improve how they work with family caregivers.
The Dementia Care Program at UCLA prepares nurse dementia care managers to provide better support to patient families and improves the coordination of care. Participants had Medicare costs that were $2,100 lower annually than a comparison group and were a third less likely to be admitted to a long-term care facility. The John A. Hartford Foundation is supporting replication of this project to benefit the millions of families in need. In addition, the RAISE Family Caregivers Act, which will lead to the development of a national strategy to recognize and support family caregivers, recently became federal law. This act was a major recommendation from The John A. Hartford Foundation-sponsored report, Families Caring for an Aging America.
The John A. Hartford Foundation doesn’t just fund things. They support and nurture the work, they seek out others who have ideas, and they help bring the best ideas to bear.
—Susan Reinhard, PhD, RN, Senior Vice President, AARP Public Policy Institute
Informing decision-makers.
In 2017, we connected federal policymakers, health system leaders, clinicians, and service providers with critical news and resources about age-friendly health care.
The Foundation is creating an environment for innovation in how our health care system responds to the needs of older Americans. We’re investing in innovative and creative minds and changing the mindset about how we provide care to older adults—for everyone from providers to family caregivers.
—David Di Martino, Partner, Blue Engine Message & Media, Trustee, The John A. Hartford Foundation

POLITICO Partnership
In September 2017, we launched a partnership with global news and information company POLITICO to connect with federal policymakers and position the Foundation as a nonpartisan resource for improving policy and practice around the care of older adults. The resulting special report, The Agenda: Aging in America, took a comprehensive deep dive into the biggest barriers to improving care for our aging population. The report coincided with a POLITICO Live event introduced by The John A. Hartford Foundation President Terry Fulmer and featured experts discussing how to make the health care delivery system more responsive to older patients with complex needs.

Kaiser Health News Reporting Project
Our partnership with Kaiser Health News builds awareness and understanding of geriatric care issues among the public, policymakers, and the health care sector. It has developed a top-tier reporting desk to inform key decision-makers and the public on the most pressing aging and geriatric care issues. This year our funding resulted in more than 120 articles, two large-scale investigative projects, and two events in Washington, DC. Kaiser Health News amplified the reach of its articles through partnerships with The Washington Post, NPR, and others, spreading awareness to thousands of additional readers.

Health Affairs Aging and Health Series
As part of our work with Health Affairs, we supported the publication and wide dissemination of research, analysis, and commentary on new health care models that improve care for older adults. Health Affairs’ reputation as the nation’s leading health policy journal advanced best practices in the care of older adults and positioned aging and health policy issues as central to the national health care dialogue. In 2017, Health Affairs completed its two-year Aging and Health series with our support, publishing 17 articles, 15 blog posts, and holding two events in Washington, DC. The series was renewed and will continue for another two years.

Congressional Stories of Family Caregiving
In November 2017, we supported a briefing on Capitol Hill where six members of the US House of Representatives—Rep. Debbie Dingell, D-MI; Rep. Michelle Lujan Grisham (pictured), D-NM; Rep. Jim Langevin, D-RI; Rep. Jacky Rosen, D-NV; Rep. Jan Schakowsky, D-IL; and Rep. Chris Smith, R-NJ called for better supports and services for family caregivers and shared their personal stories to illustrate the challenges that accompany the family caregiving experience. “Congressional Stories of Family Caregiving: Challenges, Rewards, and A Call to Action” was hosted by the Gerontological Society of America, which released a proceedings paper. Afterward, in an op-ed in The Hill, The John A. Hartford Foundation Program Director Rani Snyder lauded the efforts of 39 states and territories in enacting the CARE Act critical to families caring for older adults.