 I bet every reader of Health AGEnda knows someone who is a family caregiver (many see one every day in the mirror). And I bet every family member or friend providing care to an older adult who needs assistance because of chronic disease or frailty has their stories of good and bad days—of feeling incredibly fulfilled and completely overwhelmed.
I bet every reader of Health AGEnda knows someone who is a family caregiver (many see one every day in the mirror). And I bet every family member or friend providing care to an older adult who needs assistance because of chronic disease or frailty has their stories of good and bad days—of feeling incredibly fulfilled and completely overwhelmed.
Caregivers have much in common with each other, and our policies and systems need several overarching improvements to address caregiver needs. That is why the John A. Hartford Foundation is supporting an Institute of Medicine study to lay out the top level policy and practice recommendations (For more information, read New Grants Target Policy and Practice Change.)
However, it is worth noting that not all caregiving is the same. A recent analysis funded by the John A. Hartford Foundation from the AARP Public Policy Institute and the United Hospital Fund points to the especially difficult circumstances of those who care for people with cognitive impairment (such asAlzheimer’s or other dementias) and/or behavioral health conditions (such as depression, anxiety or serious mental illness), referred to in the study together as “challenging behaviors.”
As the study shows, caregivers of people with challenging behaviors are different from other caregivers in a number of ways. These caregivers are responsible for people who—beyond their dementia, depression, or other related condition—are just plain sicker. These care recipients have more co-occurring chronic conditions and require more ambulatory surgery services, emergency department visits, and hospitalizations.
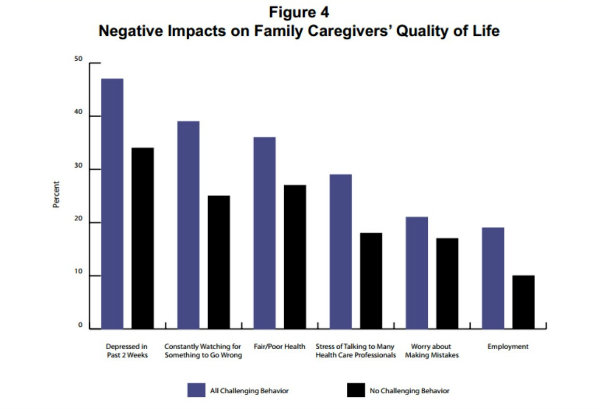
Caregivers of those with challenging behaviors are more likely than other caregivers to perform more than one complex medical/nursing task, such as managing medications or using monitors and telehealth equipment. And strikingly (and probably not surprisingly), these caregivers report much higher levels of stress and self-reported depression than other caregivers.
On the flipside, these caregivers know they are doing something special and important. Sixty percent of people caring for family members with challenging behaviors believe their efforts have allowed their loved one to remain at home and out of a nursing home. That is compared to 43 percent of those who care for adults without challenging behaviors.
So what can be done for family caregivers whose loved ones are struggling with dementia or behavioral health issues? The report authors offer a number of recommendations, including better integration of behavioral health programs into medical care, setting up special respite and adult day care programs for this group, giving these caregivers more access to evidence-based training on how to respond to challenging behaviors, and training health care providers to better work with these caregivers and their patients.
Very importantly, the report recommends that policymakers ensure that programs for people with dementia and/or behavioral health problems include support and training for family caregivers on managing the care of the whole person and not just the specific condition.
Through the Hartford Change AGEnts Initiative, a Dementia Caregiving Network of experts has formed that is working to achieve improvements in services and supports for family caregivers of persons with dementia. We hope this work will connect to and support larger national efforts and that, in combination with studies like this most recent Hartford-supported report, more attention and appropriate resources will be devoted to helping caregivers who need assistance the most.
Family Caregivers Providing Complex Chronic Care to People with Cognitive and Behavioral Health Conditions is the fourth public policy report on family caregiving in a series supported by the John A. Hartford Foundation and produced by the AARP Public Policy Institute in collaboration with the United Hospital Fund. Other reports in the series are:
