Nursing: The Key to Quality Patient Care
Until they have to learn it for themselves, often by overseeing care for their aging parents, most people don’t appreciate the many complexities of providing health care to older persons. Lack of knowledge about proper care of older adults can result in inadequate assessment, missed or erroneous diagnoses, treatments that can harm rather than heal, and a reduced quality of life. Lack of knowledge can also contribute to increased risk for complications or even death, unnecessary or prolonged hospitalization, readmissions shortly after discharge, temporary or permanent placement in nursing homes, and unnecessary increases in the cost of healthcare. Nurses trained in gerontology are prepared to meet the unique challenges of caring for older adults.
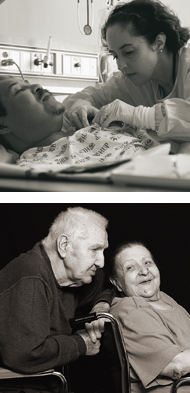
Of all the nursing specialties, geriatrics is an area where nursing skills can particularly shine. As the professionals with the most frequent direct contact with patients, nurses are in a position to detect signs and symptoms, including subtle changes in a patient’s condition, that signal the need for intervention. This can be an especially crucial function when caring for vulnerable older patients. In general, nursing skills are particularly well suited for assessing and managing chronic care of patients, both of which are essential when treating elderly patients.
In keeping with its overall goal to increase the nation's capacity to provide effective, affordable care to its rapidly increasing older population, in 1996 the John A. Hartford Foundation turned its focus for the first time to a major initiative in nursing, with a $5 million five–year grant to create the John A. Hartford Foundation Institute for Geriatric Nursing at New York University. Between 1993 and 1995, the Foundation had made significant investments in fostering the training of doctors in care of older adults, as well as supporting models to jointly train doctors, nurses, social workers and other health professionals in interdisciplinary team skills. The award to create the Hartford Institute—the second largest grant authorized by the Trustees in the Foundation's modern history—recognized the vital contribution of nurses. The Foundation also realized that, just as in medicine and social work, the curricula used for training new nurses lacked geriatric content. In addition, in-service nursing education for those already in the workforce also often failed to address geriatric content.
Although there were pockets of excellence in the field of nursing and some outstanding pioneers, ten years ago there was no national legitimacy or central catalyst for the promotion of geriatric nursing. Nurses who did specialize in geriatrics often found scant support in their work environment for initiatives to improve care of older patients. Before 1996, there were no hospital-wide initiatives to improve overall care of older patients. There was very little in the way of materials or resources to use to train staff or assess knowledge about care of older adults. There was no national initiative focused on teaching competencies in care of older adults for baccalaureate nursing students. There were no training projects to prepare faculty to teach care of older adults in baccalaureate nursing programs. There was virtually no curriculum at the baccalaureate level on geriatrics. In terms of nursing research, the primary organization for interdisciplinary geriatric research, the Gerontological Society of America (GSA), had no nursing interest group or award recognizing nursing research contributions. Finally, important public policy issues regarding nursing care for older adults were not effectively addressed.
Today, as the Hartford Institute for Geriatric Nursing celebrates ten years of dedication to promoting the highest level of geriatric competence in all nurses, profound changes have taken place in the nursing profession. In the realm of nursing education, over 90 percent of baccalaureate nursing programs now have gerontological content integrated into their curriculum. The American Association of Colleges of Nursing (AACN) has added geriatrics to its set of core competencies expected of all graduates of baccalaureate nursing programs, and because of the Hartford Institute's commitment to translating nursing science to the bedside, geriatric-focused assessment tools and best practices are now readily available to practicing nurses. Nurses who pursue an academic career now receive critical career-enhancing support and mentorship as they work to shape the future of nursing education. Nurse researchers also have unprecedented recognition and a forum for collegial exchange at the annual meeting of the GSA.At the systems level, the Hartford Institute has supported the implementation of hospital-wide practices and protocols that ensure older patients receive the highest quality care. The Hartford Institute's initiatives in this area have produced tangible results for older patients, significantly decreasing the incidence of such hospital-related complications as pressure ulcers, falls, and delirium.
Over the past ten years, the Hartford Institute has also raised the profile of geriatric nursing by creating nationally recognized awards for excellence in nursing curriculum, research, and practice, and by providing a forum for high-level policy discussions on issues that impact the entire field of geriatric nursing.
A measure of the Hartford Institute's success as an instrument of
change in the nursing profession has been its ability to leverage
Hartford Foundation funding and obtain additional support.
The funding and commitment from influential organizations will
ensure the ongoing success of the Hartford Institute's initiatives and
lead to lasting change in the field of nursing. The Hartford Institute
has had a transformative effect on nursing at all levels.
1- Thomas, Lewis. The Youngest Science: Notes
of a Medicine-Watcher. New York: Viking Press,
1983
2- Cohen HJ, Feussner JR, Weinberger M, et al.
"A Controlled Trial of Inpatient and Outpatient
Geriatric Evaluation and Management." New
England Journal of Medicine. 2002. Vol. 346,
Number 12, pp. 905-912.
Visit the Hartford Institute for Geriatric Nursing Web site: www.hartfordign.org