![]()
 Hartford Change AGEnt Zara Cooper, MD, a surgeon at Brigham and Women’s Hospital’s trauma, burns, and surgical critical care division.
Hartford Change AGEnt Zara Cooper, MD, a surgeon at Brigham and Women’s Hospital’s trauma, burns, and surgical critical care division.
A standard memory test commonly used in geriatrics practice involves asking patients to remember three objects and draw a clock. Thanks to a Hartford Change AGEnts Action Award, surgeons at Brigham and Women’s Hospital in Boston are now learning if results from this exam can help mitigate the risks among older patients for developing post-operative delirium, a sudden, dangerous, and often frightening state of confusion that is associated with increased risk of mortality and poor outcomes.
Specifically, the Action Award is supporting the development of a training video that teaches clinicians how to administer the exam, the collection of data on how much time it adds to the pre-op visit, and the documenting and measuring of how well it works.
“The Action Awards provide just the right amount of funding to kick-start clinical initiatives that otherwise probably wouldn’t happen, such as the cognitive screening we’re doing in our pre-operative assessment center. Because there’s not a lot of evidence around these kinds of initiatives thus far, it’s often hard to get financial support from your institution. Without the Change AGEnts grant, we’d never be able to get this off the ground in any kind of structured way because we wouldn’t have the money to collect the data to actually prove to our hospital that this works.”
-Zara Cooper, MD
“We want to better understand how we can implement this as part of our workflow,” says Zara Cooper, MD, the surgeon and Hartford Change AGEnt leading the project who works in the hospital’s trauma, burns and surgical critical care division.
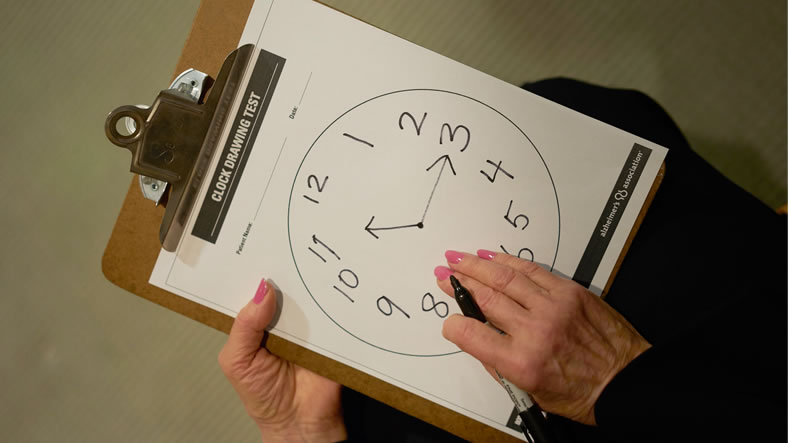 The brief Mini-Cog test is used in the Brigham and Women’s pre-op testing center to screen for unrecognized cognitive impairment that could place a patient at risk for post-operative delirium. First, a patient is asked to remember three unrelated words from a list validated in a clinical study. The patient is asked to repeat the words to ensure that she or he heard them correctly. The patient is then asked to draw the face of a clock on a sheet of paper with a large circle, filling in the numbers in the proper positions. Next, the patient is asked to draw hands on the clock for a specific time. Afterward, the patient is asked to recall the three words they were given initially. The results are then tabulated. One to two recalled words plus an abnormal clock drawing or zero recalled words is a sign of cognitive impairment at the time of the test. Further assessment may be deemed necessary..
The brief Mini-Cog test is used in the Brigham and Women’s pre-op testing center to screen for unrecognized cognitive impairment that could place a patient at risk for post-operative delirium. First, a patient is asked to remember three unrelated words from a list validated in a clinical study. The patient is asked to repeat the words to ensure that she or he heard them correctly. The patient is then asked to draw the face of a clock on a sheet of paper with a large circle, filling in the numbers in the proper positions. Next, the patient is asked to draw hands on the clock for a specific time. Afterward, the patient is asked to recall the three words they were given initially. The results are then tabulated. One to two recalled words plus an abnormal clock drawing or zero recalled words is a sign of cognitive impairment at the time of the test. Further assessment may be deemed necessary..
The Action Award project builds off a pilot study initiated by Deborah Culley, MD, an anesthesiologist at Brigham and Women’s who—like Dr. Cooper—is a former recipient of a Dennis W. Jahnigen Career Development Award. Dr. Culley found that 22 percent of geriatric patients who were given a brief cognitive screening test during their pre-op visit had unrecognized cognitive deficits. The finding is significant, Dr. Cooper says, because cognitive impairment in older patients “means they are at risk for delirium, which is associated with [bad] post-op outcomes.”
“Right now, we’re using it as a screening tool for delirium, much in the same way the cardiac stress test is a screening tool for myocardial infarctions,” she says. “It doesn’t mean you’ll have one, but it may mean you’re at high risk, and we need to look at what we can do to mitigate your risk.”
Under another pilot program separate from the Action Award grant, a patient identified with cognitive impairment can meet with a geriatrician to develop strategies to reduce the risk of post-op delirium, Dr. Cooper says. This may include monitoring medications, changing the frequency that vital signs are checked, and avoiding putting the patient in the intensive care unit, which has been found to increase the risk of post-op delirium.
As a surgeon who, by her own admission, “went into trauma to do the kind of heroic operative interventions for young people who’ve been shot,” Dr. Cooper may not seem the most likely person to lead the implementation of a geriatrics intervention. But about 50 percent of trauma admissions at Brigham and Women’s are patients over age 65, many of whom are there as the result of falls, she says.
And in addition to being board certified in surgery and surgery critical care, Dr. Cooper became certified in hospice and palliative medicine in 2012 “because I deal with a lot of patients who have very serious illnesses and are at a high risk of death.”
“My interest in geriatrics, my experience as a Hartford awardee, and my prior and ongoing collaborations with this team are what led me to spearhead this,” Dr. Cooper says. “Also, I did a prior study in the pre-op testing center for advance care planning, so I had experience conducting studies in that setting.”
It is not an easy place to do research on practice improvement. Some 25,000 patients go through the pre-op testing center each year at the Weiner Center for Preoperative Evaluation. “Because of our high volume, we see hundreds of patients a day so we can’t really prolong that visit too much,” Dr. Cooper says.
In addition to Dr. Cooper, the team working on the Action Award grant includes Dr. Culley; Houman Javedan, MD, a Hartford Center of Excellence in Geriatric Medicine and Training scholar who is director of inpatient geriatrics at Brigham and Women’s; and Angela Bader, MD, MPH, director of the Weiner Center.